Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Understand the link between diabetes and oral health and what you need to know.
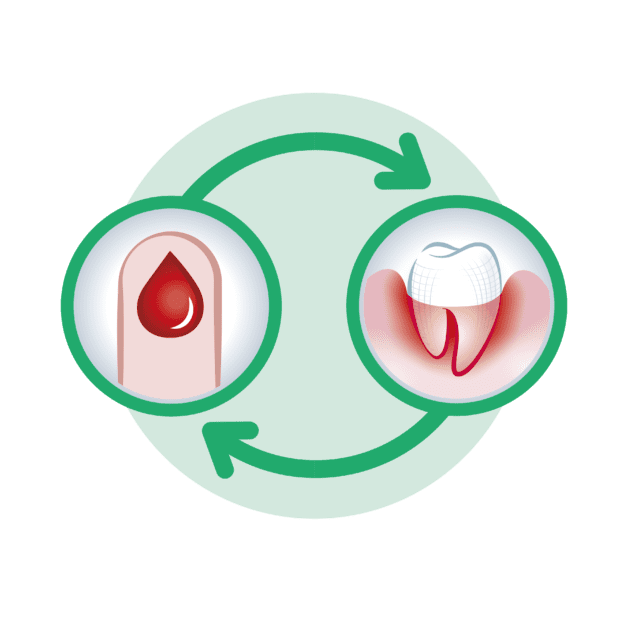
Diabetes and oral health are closely linked, with one impacting the other in various ways. Research has shown that individuals with diabetes have a higher risk of developing oral health problems, while poor oral health can also negatively affect blood sugar control in diabetics. This connection is crucial to understand, as it emphasizes the importance of comprehensive oral care for individuals with diabetes.
Scientific studies have found that individuals with diabetes are more prone to gum disease, also known as periodontal disease. This chronic inflammatory condition affects the tissues surrounding the teeth, leading to gum inflammation, gum recession, and even tooth loss if left untreated. The underlying cause of this connection lies in the impaired ability of the body to fight infections, a common characteristic of diabetes. High blood sugar levels also contribute to the development of gum disease, as they provide an ideal environment for bacteria to thrive in the mouth. Additionally, gum disease can further complicate blood sugar control in diabetics, creating a cycle of increased vulnerability to oral health problems.
Alongside gum disease, tooth decay is another oral health issue that can be influenced by diabetes. Research has suggested that individuals with diabetes may have a higher incidence of cavities compared to those without diabetes. This can be attributed to several factors, including decreased saliva production, which reduces the natural cleansing and protective properties of saliva. Moreover, the consumption of sugary foods or beverages to manage hypoglycemia or satisfy cravings can contribute to tooth decay. Dental professionals play a crucial role in educating individuals with diabetes about the importance of maintaining good oral hygiene and following a healthy diet to prevent tooth decay.
Understanding the connection between diabetes and oral health is essential for both healthcare professionals and individuals with diabetes themselves. By recognizing the increased risks and possible complications, individuals with diabetes can take proactive steps to prioritize their oral health. Regular dental check-ups, consistent oral hygiene practices, and coordinated care between dentists and endocrinologists can all contribute to better oral health outcomes for individuals with diabetes. Empowering individuals with knowledge about the link between diabetes and oral health empowers them to take charge of their overall well-being.

Gum disease, also known as periodontal disease, is a common oral health condition that affects the soft tissues and bones supporting the teeth. Numerous studies have highlighted the strong connection between diabetes and gum disease, revealing that individuals with diabetes are at a higher risk for developing this oral health condition.
One of the primary reasons for this link is the impact of diabetes on the body’s immune system. Diabetes compromises the body’s ability to fight off infections, including those in the gums. Consequently, individuals with diabetes have a weakened immune response, making them more susceptible to gum disease. Moreover, uncontrolled blood sugar levels can lead to increased levels of glucose in the saliva, providing a fertile breeding ground for harmful bacteria that contribute to gum inflammation and infection.
Aside from compromising the body’s immune system, diabetes can also affect the blood vessels, leading to decreased blood flow to the gums. This reduced blood circulation impairs the mouth’s natural healing process, making it more challenging for gum tissues to repair themselves and recover from infection. Additionally, studies have shown that the presence of gum disease can further exacerbate diabetes by making it more challenging to control blood sugar levels. This creates a vicious cycle, as uncontrolled diabetes can worsen gum disease, and vice versa.
In light of these findings, it becomes crucial for individuals with diabetes to prioritize their oral health. Maintaining good blood sugar control through appropriate diet, exercise, and medication can significantly reduce the risk and severity of gum disease. Additionally, establishing a thorough oral hygiene routine, which includes regular brushing, flossing, and professional dental cleanings, is essential in preventing and managing gum disease. By taking proactive steps to address the impact of diabetes on gum disease, individuals can safeguard their oral health and overall well-being.
| Aspect | Impact of Diabetes on Gum Disease |
|---|---|
| Increased Risk | Diabetes increases the risk of developing gum disease (periodontitis) due to elevated blood sugar levels, which can weaken the body’s ability to fight infections, including those in the gums. |
| Severity | Diabetic individuals are more prone to experiencing severe forms of gum disease compared to non-diabetics. |
| Progression | Gum disease tends to progress more rapidly and aggressively in people with diabetes, leading to potential complications such as tooth loss and gum tissue damage. |
| Response to Treatment | Diabetic patients may respond less effectively to treatment for gum disease, and healing processes can be slower due to compromised immune function and impaired circulation associated with diabetes. |
| Complications | Uncontrolled gum disease in diabetic individuals can exacerbate blood sugar levels, making diabetes harder to manage. Conversely, uncontrolled diabetes can worsen gum disease, creating a vicious cycle of complications. |
Tooth decay, also known as dental caries, is a common oral health issue that affects people of all ages. However, research has shown a clear link between diabetes and an increased risk of tooth decay. Understanding this relationship is crucial for individuals with diabetes in order to effectively manage their oral health.
When it comes to tooth decay, the primary culprit is the presence of harmful bacteria in the mouth. These bacteria thrive on sugars and carbohydrates found in food and produce acids that erode the protective layer of the teeth, eventually leading to cavities. In individuals with diabetes, the elevated levels of glucose in the saliva provide an ideal environment for these bacteria to flourish, increasing the likelihood of tooth decay.
Furthermore, diabetes can also affect the body’s ability to heal and fight off infections, including those in the mouth. This compromised immune response can make it more difficult for the body to combat the bacteria that cause tooth decay. As a result, individuals with diabetes may experience more severe and rapid tooth decay compared to those without diabetes.
In addition to proper oral hygiene practices such as brushing and flossing regularly, individuals with diabetes should prioritize blood sugar control as a means of preventing tooth decay. By maintaining stable blood sugar levels, the amount of glucose in saliva can be minimized, reducing the food source for bacteria in the mouth. This, in turn, decreases the risk of tooth decay and promotes better overall oral health.
Overall, exploring the relationship between diabetes and tooth decay highlights the importance of proactive dental care for individuals living with diabetes. By understanding the risk factors and implementing strategies to prevent tooth decay, individuals with diabetes can maintain optimal oral health and minimize the potential complications associated with their condition.
Oral health complications are a common concern among individuals with diabetes. The interplay between diabetes and oral health can lead to various issues, ranging from gum disease to tooth decay. Diabetes affects the body’s ability to control blood sugar levels, which can have a significant impact on oral health. Studies have shown that individuals with diabetes are more prone to gum disease, also known as periodontitis, than those without diabetes. This is because diabetes weakens the body’s immune system, making it harder to fight off infections in the gums. As a result, gum disease progresses more rapidly in diabetic individuals, leading to symptoms such as swollen gums, bleeding, and receding gum lines.
In addition to gum disease, tooth decay is also a prevalent complication in individuals with diabetes. The high levels of glucose in the saliva of diabetic individuals create an ideal environment for bacteria to thrive, leading to the formation of plaque and tooth decay. Poor blood sugar control further exacerbates this concern, as high glucose levels can negatively affect the tooth’s ability to fight off acid-producing bacteria. Consequently, diabetic individuals may experience an increased risk of cavities and tooth loss.
Considering the potential oral health complications associated with diabetes, it is crucial for individuals with this condition to prioritize their dental care. Regular dental check-ups and professional cleanings are essential to monitor and address any oral health issues promptly.
Maintaining good oral hygiene, such as brushing twice a day, flossing, and using antimicrobial mouthwashes, is vital in preventing gum disease and tooth decay. Moreover, proper blood sugar management is fundamental in reducing the risk and severity of oral health complications. By working closely with both their dentist and endocrinologist, individuals with diabetes can develop a comprehensive treatment plan that addresses the unique challenges posed by this condition. With proper management and care, individuals with diabetes can maintain optimal oral health and reduce the risk of complications.

The management of diabetes plays a crucial role in maintaining optimal oral health. Individuals with diabetes have an increased risk of developing various oral health complications, including gum disease, tooth decay, and fungal infections. Therefore, it is essential for diabetic individuals to prioritize the management of their diabetes to achieve better oral health outcomes.
One of the key aspects of managing diabetes for better oral health is maintaining stable blood sugar levels. High blood sugar levels can weaken the immune system and impair the body’s ability to fight off bacteria and infections, including those in the mouth. By closely monitoring blood sugar levels and following a diabetes management plan, individuals can lower their risk of developing oral health complications.
Additionally, regular dental visits are crucial for individuals with diabetes. Dentists can assess their oral health status, identify any early signs of complications, and provide necessary treatments. Moreover, dental professionals can offer personalized oral care tips and techniques to maintain optimal oral hygiene.
By taking proactive measures to manage diabetes effectively and maintain good oral hygiene, individuals can significantly reduce the risk of oral health complications. It is important for individuals with diabetes to collaborate with their healthcare team, including dentists and endocrinologists, to develop a comprehensive management plan that addresses both their diabetes and their oral health needs. Together, optimal diabetes management and good oral hygiene practices can contribute to improved overall health and well-being.
Maintaining blood sugar control is crucial for overall health, including dental care. Consistently high blood sugar levels can have a significant impact on oral health, increasing the risk of developing various dental problems. Poor blood sugar control can weaken the body’s immune system, making it more difficult to fight off infections, including those that affect the gums and teeth.
One of the most common oral health complications associated with diabetes is gum disease. When blood sugar levels are high, the risk of gum disease, also known as periodontal disease, is significantly higher. This is because high blood sugar levels can lead to increased plaque buildup and inflammation in the gums, making them more susceptible to bacterial infections. In turn, gum disease can further worsen blood sugar control, creating a vicious cycle. It is essential for individuals with diabetes to take proactive measures to manage their blood sugar levels to minimize the risk of gum disease and other oral health complications.
| Aspect | Importance/Impact |
|---|---|
| Gum Disease Risk | – High blood sugar increases the risk of gum disease |
| – Poorly controlled diabetes can lead to gum infections | |
| Tooth Decay | – Elevated blood sugar contributes to tooth decay |
| – Increased risk of cavities and dental caries | |
| Healing | – Slower healing in the mouth with uncontrolled blood sugar |
| – Delayed recovery from dental procedures | |
| Oral Infections | – Elevated blood sugar weakens the immune system, leading to increased susceptibility to oral infections |
| Periodontal Health | – Blood sugar control is crucial for maintaining periodontal health |
| – Helps in preventing and managing periodontal disease |
Diabetes is a condition that affects the body’s ability to regulate blood sugar levels, which can lead to various health complications. One area that is particularly vulnerable in diabetic individuals is oral health. Recognizing the symptoms of oral health issues in diabetic patients is crucial in order to address and manage these problems effectively.
One common oral health issue that diabetic individuals may experience is gum disease, also known as periodontal disease. Symptoms of gum disease include redness, swelling, and bleeding gums, as well as bad breath and loose teeth. Diabetic patients may be more prone to gum disease due to their compromised immune system and reduced ability to fight off infections. Thus, it is important for dentists to educate their diabetic patients about the early signs of gum disease and emphasize the need for regular dental check-ups and professional cleanings to prevent its progression.
Another symptom that diabetic individuals should be mindful of is dry mouth, also known as xerostomia. This condition occurs when there is insufficient saliva production, leading to a dry and uncomfortable feeling in the mouth. Dry mouth can increase the risk of tooth decay and oral infections. Diabetic patients may experience dry mouth as a side effect of certain medications or as a result of poorly managed blood sugar levels. It is crucial for dentists to inquire about any dry mouth symptoms during dental visits and provide guidance on proper oral hygiene practices and the use of saliva substitutes if necessary.
Recognizing the symptoms of oral health issues in diabetic patients is crucial for early intervention and effective management. Regular dental check-ups and open communication between dentists and diabetic individuals can help prevent the progression of oral health complications and promote better overall oral health.
Maintaining good oral health is crucial for individuals with diabetes, as they are more susceptible to developing oral health complications. By taking preventive measures and adopting a diligent oral care routine, individuals with diabetes can effectively protect their oral health. Regular brushing and flossing are fundamental practices that can help prevent tooth decay and gum disease. It is recommended to brush at least twice a day with a soft-bristled toothbrush and fluoride toothpaste, paying special attention to the gumline and all tooth surfaces. Flossing once a day helps remove plaque and food particles from areas that your toothbrush cannot reach, reducing the risk of gum disease.
In addition to brushing and flossing, individuals with diabetes should also make healthy lifestyle choices to protect their oral health. Eating a balanced diet that is low in sugars and high in vitamins and minerals can promote strong teeth and gums. Regular exercise and proper management of blood sugar levels are important not only for overall health but also for maintaining good oral health. High blood sugar levels can contribute to dry mouth, which increases the risk of tooth decay and other oral health issues. By working closely with their healthcare team, individuals with diabetes can manage their blood sugar levels effectively, reducing the potential impact on their oral health.
Regular dental check-ups are crucial for individuals with diabetes to maintain optimal oral health. Diabetes can significantly increase the risk of developing oral health conditions such as gum disease and tooth decay. However, with regular dental check-ups, potential issues can be detected early, allowing for prompt intervention and successful management.
During dental check-ups, dentists can thoroughly examine the mouth for any signs of gum disease or tooth decay. They can evaluate the gum tissues, measure the depth of periodontal pockets, and assess the integrity of the teeth. This comprehensive assessment enables dentists to identify any areas of concern and provide appropriate treatment recommendations. Regular check-ups also provide an opportunity for dentists to educate diabetic individuals on proper oral hygiene practices and offer personalized advice for managing their condition effectively. By working closely with both patients and their healthcare providers, dentists play a vital role in the overall well-being of individuals with diabetes, ensuring that any potential oral health complications are addressed promptly and appropriately.
Dentists and endocrinologists play crucial roles in managing diabetes and its impact on oral health. The collaboration between these two medical professionals is essential for providing comprehensive care to diabetic individuals.
While dentists focus on diagnosing and treating oral health issues, endocrinologists specialize in managing diabetes and its related complications. By working together, dentists and endocrinologists can develop personalized treatment plans that address both the dental and medical aspects of diabetes. This collaboration allows for a holistic approach to diabetes management, considering factors such as blood sugar control, medication interactions, and overall health status.
By sharing information and coordinating care, dentists and endocrinologists can ensure that the treatment plans are aligned and optimize the overall health of their patients. This collaboration also allows for timely intervention and prevention of potential oral health complications in diabetic individuals. Regular communication between the two medical professionals enables them to identify systemic risk factors and adjust treatment plans accordingly, promoting better oral health outcomes for patients with diabetes. The collaboration between dentists and endocrinologists is crucial for comprehensive diabetes management, ensuring that patients receive the best possible care for their oral and overall health.
Maintaining good oral care is essential for individuals with diabetes to prevent oral health complications. Here are some tips to help diabetic individuals take care of their oral health:
1. Control your blood sugar levels: Keeping your blood sugar levels under control is crucial for managing diabetes and maintaining good oral health. High blood sugar levels can lead to an increased risk of gum disease and tooth decay. Work closely with your healthcare team to monitor and manage your blood sugar levels effectively.
2. Practice proper oral hygiene: Brush your teeth at least twice a day using a soft-bristled toothbrush and fluoride toothpaste. Don’t forget to clean your tongue as well. Incorporate flossing into your daily routine to remove plaque and food particles from between your teeth. Consider using an antimicrobial mouthwash recommended by your dentist to further protect your oral health.
Remember, individuals with diabetes may be more prone to oral health issues, so it’s important to prioritize your oral care. Regular dental check-ups and professional cleanings are also essential for early detection and treatment of any oral health problems. By following these oral care tips, you can help maintain a healthy smile and overall well-being.
Inflammation plays a crucial role in both diabetes and oral health. When it comes to diabetes, chronic inflammation is a key factor in the development and progression of the disease. Inflammation disrupts the body’s ability to regulate blood sugar levels, leading to insulin resistance and increased risk of Type 2 diabetes. This inflammatory response can also contribute to the development of complications associated with diabetes, including cardiovascular disease, kidney problems, and nerve damage.
In the context of oral health, inflammation is closely linked to gum disease, also known as periodontal disease. This condition occurs when plaque (a sticky film of bacteria) builds up on the teeth and irritates the gums, causing inflammation. In response to this inflammation, the body’s immune system releases substances that can damage the gums and underlying bone structure, leading to tooth loss if left untreated. Interestingly, this cycle of inflammation in the mouth can also have a negative impact on diabetes control, as it can make it harder for individuals with diabetes to manage their blood sugar levels effectively.
Understanding the role of inflammation in both diabetes and oral health is essential for effective management and prevention of complications. By addressing inflammation through strategies such as maintaining good oral hygiene, controlling blood sugar levels, and seeking regular dental care, individuals with diabetes can reduce their risk of developing gum disease and other oral health issues. Likewise, managing diabetes through lifestyle modifications, medication, and appropriate healthcare can help mitigate the chronic inflammation associated with the disease and improve overall well-being.
Diabetes is a chronic condition that affects millions of people worldwide. While the impact of diabetes on various aspects of health is well-documented, the connection between diabetes and oral health is often overlooked. It is crucial to recognize the importance of education and awareness in managing diabetes and maintaining good oral health.
Individuals with diabetes are more prone to developing gum disease, also known as periodontal disease. This is due to the impaired ability to control blood sugar levels, which can weaken the immune system and increase the risk of infection. Furthermore, gum disease can also affect blood sugar control, creating a vicious cycle that can worsen both diabetes and oral health.
In addition to gum disease, individuals with diabetes are also at a higher risk of experiencing tooth decay. The elevated sugar levels in the saliva provide an ideal environment for bacteria to thrive, leading to the formation of plaque and cavities. It is essential for diabetic individuals to understand the connection between diabetes and tooth decay and take preventive measures, such as maintaining a good oral hygiene routine and making regular visits to the dentist.
Education and awareness play a crucial role in preventing and managing oral health complications in diabetic individuals. By understanding the potential risks associated with diabetes and how it can impact oral health, individuals can take proactive steps to protect their teeth and gums. Regular dental check-ups, proper oral hygiene practices, and blood sugar control are essential components of a comprehensive dental care plan for diabetic patients.
By empowering diabetic individuals with knowledge and resources, we can improve their oral health outcomes and overall quality of life. Dental professionals, along with healthcare providers specializing in diabetes management, can work collaboratively to educate patients about the importance of oral health and provide tailored recommendations and treatment plans.
In conclusion, education and awareness are instrumental in managing diabetes and maintaining optimal oral health. By understanding the connection between diabetes and oral health complications, individuals can take proactive steps to prevent gum disease and tooth decay. Dental professionals and healthcare providers have a vital role in conveying this knowledge and providing comprehensive care to diabetic patients. Together, we can strive for better oral health outcomes for those living with diabetes.
Diabetes can significantly impact oral health. Individuals with diabetes are more prone to gum disease and tooth decay due to high blood sugar levels.
Diabetes weakens the body’s ability to fight off bacteria, making diabetic individuals more susceptible to gum disease. It can also worsen existing gum disease and slow down the healing process.
Yes, diabetes can increase the risk of tooth decay. High blood sugar levels provide an ideal environment for the growth of harmful bacteria in the mouth, leading to tooth decay.
Diabetic individuals may experience dry mouth, oral infections, slow healing of oral tissues, burning mouth syndrome, and an increased risk of oral thrush.
Proper management of diabetes, including maintaining stable blood sugar levels, can help reduce the risk and severity of oral health issues.
Good blood sugar control is crucial for diabetic individuals, as it promotes better overall oral health and aids in the prevention and management of oral health complications.
Diabetic patients should be vigilant about symptoms such as persistent bad breath, swollen or bleeding gums, loose teeth, dry mouth, and mouth ulcers, as these may indicate oral health issues.
Diabetic individuals should maintain good oral hygiene practices, such as brushing and flossing regularly, avoiding sugary foods and drinks, and quitting smoking.
It is recommended that diabetic individuals visit their dentist for regular check-ups and cleanings every six months to monitor their oral health and address any concerns promptly.
Collaboration between dentists and endocrinologists is essential to ensure comprehensive diabetes management. It allows for a holistic approach that considers both the oral health and overall health of diabetic individuals.
Diabetic individuals should use a soft-bristle toothbrush, brush gently but thoroughly, clean dentures daily, use alcohol-free mouthwash, and maintain a balanced diet to support oral health.
Inflammation is a common factor in both diabetes and oral health issues. Uncontrolled inflammation can worsen diabetes symptoms and contribute to the progression of oral health complications.
Education and awareness empower individuals with diabetes to understand the connection between their condition and oral health. By recognizing the importance of proper oral care, they can take proactive measures to prevent and manage oral health issues effectively.