Table of Contents
Signs and Symptoms of Gum Disease
Gum disease, medically known as periodontal disease, is a common oral health issue that affects the tissues surrounding the teeth. Recognizing the signs and symptoms of gum disease is crucial for early intervention and effective treatment. One of the primary indicators of gum disease is bleeding gums, especially during brushing or flossing. Persistent bad breath or a bad taste in the mouth can also point towards gum disease. Additionally, gums that appear red, swollen, or receding are often early signs of underlying periodontal problems.

As gum disease progresses, you may experience increased tooth sensitivity, loose teeth, and the formation of pockets between the gums and teeth. These pockets can harbor bacteria and contribute to further deterioration of the gum tissue and underlying bone structure. Chronic inflammation in the gums, along with pain or discomfort while chewing, are also common symptoms of advanced gum disease. It is essential to pay attention to these warning signs and seek professional dental care to prevent the escalation of gum disease and safeguard your oral health in the long term.
Causes of Gum Disease
Gum disease, also known as periodontal disease, is a common condition that affects the gums and surrounding tissues. The primary cause of gum disease is the buildup of plaque, a sticky film of bacteria that forms on the teeth. When plaque is not adequately removed through proper oral hygiene practices like brushing and flossing, it can harden into tartar, leading to gum inflammation and irritation.
Additionally, factors such as smoking, hormonal changes, diabetes, certain medications, and genetic predisposition can also contribute to the development of gum disease. Poor nutrition and a diet high in sugars and carbohydrates can further exacerbate the risk of gum disease. Understanding these causes is crucial in taking preventive measures to maintain optimal oral health and prevent the progression of gum disease.
Table
| Cause | Prevention |
|---|---|
| Poor oral hygiene | Regular brushing and flossing |
| Smoking or tobacco use | Quitting smoking/tobacco |
| Diabetes | Managing blood sugar levels |
| Medications that reduce saliva | Regular dental check-ups |
| Genetic susceptibility | Early detection and treatment |
| Hormonal changes (e.g., pregnancy) | Extra dental care during hormonal changes |
| Poor nutrition | Balanced diet rich in vitamins |
Risk Factors for Gum Disease
Gum disease, also known as periodontal disease, is a common yet preventable oral health issue that can lead to serious complications if left untreated. Several risk factors can increase an individual’s susceptibility to developing gum disease, including poor oral hygiene habits, smoking, certain medical conditions, hormonal changes, genetics, and age.
Inadequate brushing and flossing can allow plaque to build up on the teeth and gums, leading to inflammation and the onset of gum disease. Smoking or using tobacco products not only weakens the immune system, making it harder to fight off bacterial infections, but also restricts blood flow to the gums, impairing their ability to heal.
Medical conditions such as diabetes, autoimmune diseases, and hormonal changes during pregnancy or menopause can also heighten the risk of gum disease by affecting the body’s inflammatory response and ability to ward off infections. Furthermore, genetics play a role in determining an individual’s susceptibility to gum disease, with some people being more genetically predisposed to developing this condition. Age is another factor, as older adults are more prone to gum disease due to the cumulative effects of poor oral hygiene habits over time and the natural thinning of gum tissues.
Stages of Gum Disease
Gum disease progresses through different stages, each signifying a varying degree of severity and damage to the oral tissues. The initial stage is gingivitis, characterized by red, swollen, and bleeding gums caused by bacterial plaque buildup along the gumline. Without proper treatment, gingivitis can advance to periodontitis, where the infection spreads deeper into the tissues and bone supporting the teeth. In advanced periodontitis, the bone loss is extensive, leading to loose teeth and potential tooth loss.
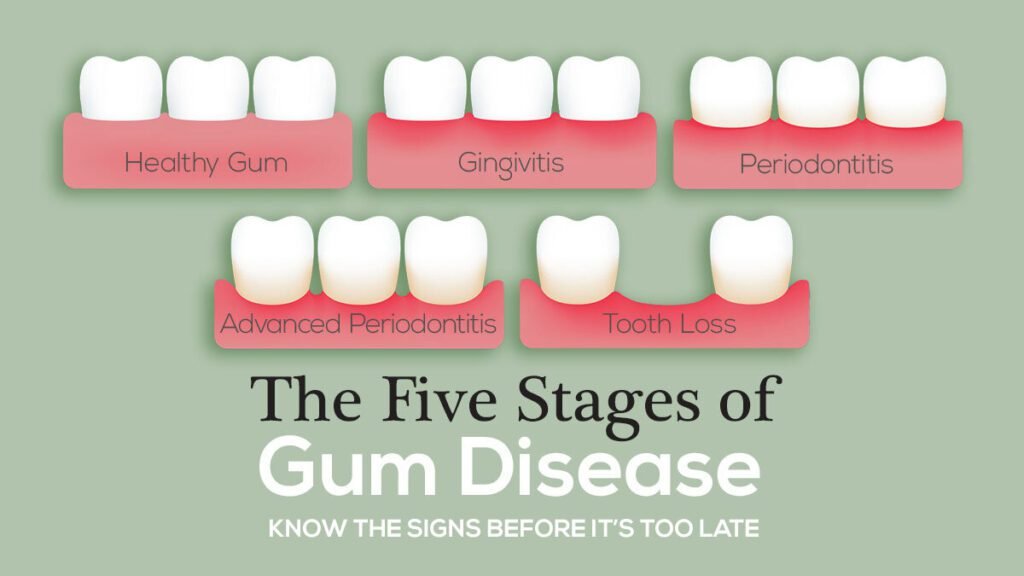
During the stages of gum disease, the body’s immune response triggers inflammation in an attempt to combat the infection. However, this chronic inflammation can ultimately damage the surrounding gum tissue and bone structure, contributing to the progression of the disease. Monitoring the signs and symptoms of gum disease and seeking early intervention from a dental professional is crucial in preventing the advancement of the condition and preserving oral health.
Prevention of Gum Disease
To prevent gum disease, it is crucial to maintain a diligent oral hygiene routine. This includes brushing your teeth at least twice a day with a fluoride toothpaste, flossing daily to remove plaque between teeth, and using an antimicrobial mouthwash to help reduce bacteria in the mouth. Regular visits to your dentist for professional cleanings and check-ups are also essential in preventing gum disease. Additionally, adopting a healthy diet low in sugary and acidic foods can help protect your gums from inflammation and infection.
Incorporating habits like quitting smoking and managing stress can also contribute to preventing gum disease. Smoking is a significant risk factor for gum disease as it weakens the immune system and hampers the body’s ability to fight infections. Stress, on the other hand, can lead to behaviors like teeth grinding and clenching, which can put added pressure on the gums and teeth. By making conscious efforts to maintain good oral hygiene practices and address lifestyle factors that can impact gum health, you can significantly reduce your risk of developing gum disease.
Importance of Regular Dental Check-ups
Regular dental check-ups are essential for maintaining optimal oral health and preventing various dental issues, including gum disease. During these routine visits, your dentist will thoroughly examine your teeth and gums, looking for any signs of infection, inflammation, or other problems that could indicate the presence of gum disease. Additionally, professional cleanings performed by a dental hygienist help remove plaque and tartar buildup, which are major contributors to gum disease development.

These check-ups also provide an opportunity for your dentist to assess your overall oral hygiene practices and make recommendations for improvement. By attending regular dental appointments, you can catch gum disease in its early stages when it is more easily treatable and prevent further progression that may lead to serious complications. Prioritizing regular dental check-ups is a proactive step towards ensuring a healthy smile and overall well-being.
Impact of Gum Disease on Overall Health
Gum disease, also known as periodontal disease, is not only a threat to oral health but can also have significant implications for overall well-being. Research has shown that the inflammation and bacteria associated with gum disease can enter the bloodstream, leading to systemic health issues. For instance, untreated gum disease has been linked to conditions such as heart disease, diabetes, respiratory infections, and even complications during pregnancy.
Moreover, the chronic inflammatory response triggered by gum disease can exacerbate existing health conditions, making it crucial to address periodontal issues promptly. Studies have also suggested a potential bidirectional relationship between gum disease and certain systemic illnesses, reinforcing the importance of maintaining good oral hygiene practices and seeking regular dental care to safeguard both oral and overall health.
Treatment Options for Gum Disease
Gum disease, also known as periodontal disease, can progress from mild gingivitis to severe periodontitis if left untreated. For effective management, treatment options aim to address the infection and inflammation in the gums. One common treatment is scaling and root planing, a deep cleaning procedure that removes plaque and tartar from below the gumline and smoothens the roots to promote gum reattachment and prevent future bacterial growth. This procedure is typically performed under local anesthesia to ensure patient comfort and effectiveness.
Table
| Stage | Treatment |
|---|---|
| Gingivitis | Professional cleaning, improved oral hygiene practices |
| Slight Periodontal Disease | Scaling and root planing, possibly antibiotics |
| Moderate Periodontal Disease | Scaling and root planing, antibiotics, and potentially surgical intervention |
| Advanced Periodontal Disease | Flap surgery, bone and tissue grafts, and advanced periodontal therapy |
In cases of advanced gum disease where pockets have formed and bone loss has occurred, surgical interventions such as flap surgery or bone grafts may be necessary to repair the damage and restore gum health. These procedures are aimed at reducing pocket depths, eliminating bacteria, and promoting gum tissue regeneration. Following treatment, patients are often advised to maintain good oral hygiene practices, attend regular dental check-ups, and possibly use adjunctive therapies like antimicrobial mouth rinses to prevent recurrence of gum disease.
Professional Dental Cleanings for Gum Disease Prevention
Regular professional dental cleanings are essential for preventing gum disease. These cleanings, typically performed by a dental hygienist, involve the removal of plaque and tartar buildup that cannot be effectively addressed with regular brushing and flossing alone. The thorough cleaning helps in preventing the progression of gum disease by eliminating the bacteria that contribute to its development.
During a professional dental cleaning, the hygienist will also perform a thorough examination of your gums, looking for any signs of inflammation or infection. Early detection of gum disease is crucial for successful treatment and prevention of further complications. Additionally, the hygienist will offer guidance on proper oral hygiene techniques and provide personalized recommendations to help maintain healthy gums between visits.
Home Care Tips for Gum Disease Prevention
Maintaining good oral hygiene is crucial in preventing gum disease, a common yet preventable oral health issue. Home care plays a significant role in keeping your gums healthy. One essential tip is to brush your teeth twice a day with a fluoride toothpaste, ensuring thorough cleaning of all surfaces, including along the gumline. Additionally, flossing daily is vital to remove plaque and debris from between teeth where a toothbrush cannot reach.
Incorporating an antimicrobial mouthwash into your daily routine can help reduce bacteria that cause gum disease. Furthermore, using interdental brushes or water flossers can effectively clean areas that are difficult to reach with traditional floss. Remember, consistency is key in maintaining good oral hygiene and preventing gum disease.
Complications of Untreated Gum Disease
Untreated gum disease can lead to a range of serious complications that extend beyond the oral cavity. When the early signs of gum disease, such as gingivitis, are ignored, the condition can progress to periodontitis, causing irreversible damage to the gums, bone, and surrounding tissues that support the teeth. As the infection spreads, pockets form between the gums and teeth, allowing harmful bacteria to thrive and further exacerbate the inflammatory response in the body. This chronic inflammation not only deteriorates the oral structures but can also contribute to systemic health issues.
One of the most concerning complications of untreated gum disease is its association with an increased risk of cardiovascular disease. The inflammation triggered by gum disease can enter the bloodstream, potentially leading to the formation of plaque in the arteries and atherosclerosis. This connection highlights the far-reaching impact of oral health on overall well-being and emphasizes the importance of addressing gum disease promptly to safeguard not only dental health but also cardiovascular health.
Relationship Between Gum Disease and Heart Health
Gum disease, scientifically known as periodontal disease, has been increasingly linked to various systemic health issues, including heart disease. Research suggests that the bacteria and inflammation associated with gum disease can enter the bloodstream and potentially contribute to the development of cardiovascular problems. The exact mechanisms linking gum disease and heart health are still being explored, but it is believed that the chronic inflammation triggered by periodontal disease may play a role in damaging blood vessels and increasing the risk of heart disease.
Studies have shown that individuals with gum disease are more likely to have heart disease compared to those with healthy gums. While further research is needed to fully understand the relationship between the two conditions, healthcare professionals emphasize the importance of maintaining good oral hygiene and seeking regular dental care to not only protect dental health but also potentially reduce the risk of heart-related complications. By addressing gum disease promptly and effectively, individuals may help safeguard their heart health as well.
The Role of Genetics in Gum Disease
The role of genetics in gum disease is a fascinating area of study within the field of oral health. Research has shown that genetics can play a significant role in an individual’s susceptibility to developing gum disease. Certain genetic factors can influence the immune response in the gums, making some people more prone to inflammation and infection, which are key components of gum disease.
Studies have identified specific genetic variations that can increase the risk of gum disease. These variations can affect how the body responds to the bacteria that cause gum inflammation, ultimately impacting the progression and severity of the disease. Understanding the genetic predisposition to gum disease can help in developing personalized prevention and treatment strategies to effectively manage oral health and reduce the risk of developing gum disease.
Connection Between Gum Disease and Diabetes
Gum disease and diabetes share a bidirectional relationship, each influencing the other in potentially harmful ways. Individuals with diabetes are more prone to developing gum disease due to impaired immune function and reduced ability to fight off bacteria. Conversely, gum disease can exacerbate diabetes by causing fluctuations in blood sugar levels, making it harder for individuals to manage their condition effectively.
Moreover, inflammation is a common denominator in both conditions. The chronic inflammation seen in gum disease can worsen insulin resistance and lead to poor glycemic control in individuals with diabetes. Conversely, uncontrolled blood sugar levels in diabetes can weaken the body’s ability to combat infections, including bacterial growth in the mouth that contributes to gum disease. Therefore, it is crucial for individuals with diabetes to prioritize their oral health and work closely with both their dentist and healthcare provider to manage these intertwined conditions effectively.
Maintaining Good Oral Hygiene to Prevent Gum Disease
To maintain good oral hygiene and prevent gum disease, it is crucial to establish a consistent dental care routine. Brushing your teeth at least twice a day with fluoride toothpaste helps remove plaque buildup that can lead to gum disease. Additionally, flossing daily is essential for cleaning between teeth and along the gumline, where brushing alone may not reach. Using an antimicrobial mouthwash can also aid in reducing bacteria in the mouth, further promoting gum health.
Incorporating a balanced diet rich in vitamins and minerals is important for overall oral health. Sugary and sticky foods can contribute to plaque formation, so limiting these items can lower the risk of gum disease. Drinking plenty of water throughout the day helps wash away food particles and bacteria, keeping the mouth clean. Lastly, regular dental check-ups and professional cleanings are essential for early detection and treatment of any gum disease issues. By following these practices consistently, individuals can significantly reduce the likelihood of developing gum disease and maintain optimal oral health.
How can I tell if I have gum disease?
Common signs and symptoms of gum disease include red, swollen, or tender gums, bleeding while brushing or flossing, persistent bad breath, receding gums, and loose teeth.
What are some risk factors for developing gum disease?
Risk factors for gum disease include poor oral hygiene, smoking, hormonal changes (such as during pregnancy or menopause), diabetes, certain medications, and genetic predisposition.
How often should I visit the dentist to prevent gum disease?
It is recommended to visit the dentist for regular check-ups and cleanings at least twice a year to help prevent gum disease and catch any issues early on.
Can gum disease impact my overall health?
Yes, gum disease has been linked to various health issues such as heart disease, diabetes, respiratory infections, and complications during pregnancy. Maintaining good oral hygiene is important for overall health.
What treatment options are available for gum disease?
Treatment for gum disease may include professional dental cleanings, scaling and root planing, antibiotics, and in severe cases, surgery. It is important to consult with a dentist for the best treatment plan.
How can genetics play a role in gum disease?
Genetics can make some individuals more susceptible to gum disease. If you have a family history of gum disease, it is important to be extra vigilant about maintaining good oral hygiene and visiting the dentist regularly.
Is there a connection between gum disease and diabetes?
Yes, there is a bidirectional relationship between gum disease and diabetes. Poorly managed diabetes can increase the risk of gum disease, and gum disease can make it more difficult to control blood sugar levels. Proper oral hygiene is crucial for individuals with diabetes.
What are some complications that can arise from untreated gum disease?
Untreated gum disease can lead to tooth loss, bone damage, and even systemic health issues such as heart disease and respiratory infections. It is important to address gum disease promptly to prevent these complications.












