Table of Contents
What is Temporomandibular Joint Disorder (TMD)?
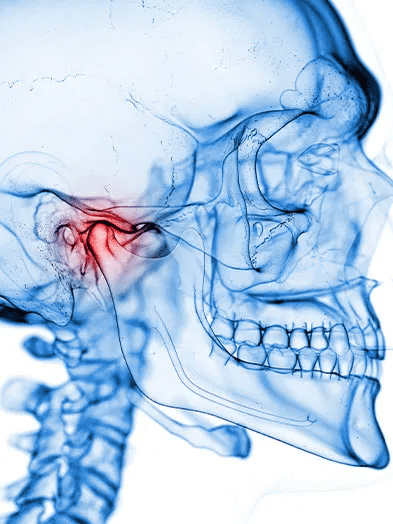
Temporomandibular Joint Disorder (TMD), also known as TMJ disorder, is a condition that affects the temporomandibular joint, which connects the jawbone to the skull. This joint is responsible for jaw movement, allowing us to speak, chew, and yawn. TMD occurs when there is dysfunction or damage to the temporomandibular joint, resulting in pain and discomfort.
TMD can manifest in a variety of ways, with symptoms ranging from mild to severe. Common symptoms include jaw pain, facial pain, headaches, difficulty in opening or closing the mouth, clicking or popping sounds when chewing, and ear pain. These symptoms can significantly impact a person’s quality of life, making it difficult to eat, speak, and perform daily activities comfortably.

It is important to note that TMD can have various causes, including jaw injury, arthritis, teeth grinding (bruxism), poor posture, and even stress. While the exact cause of TMD may be difficult to determine in some cases, seeking professional help from a dentist or a TMJ specialist is crucial for an accurate diagnosis and effective management of the disorder.
The anatomy and function of the temporomandibular joint (TMJ)
The temporomandibular joint (TMJ) is a complex hinge joint that connects the lower jawbone (mandible) to the skull. It plays a crucial role in various functions of the mouth, including chewing, speaking, and swallowing. The TMJ is located just in front of the ears, on either side of the face, and is responsible for facilitating jaw movements, such as opening and closing, as well as side-to-side and forward-backward motions.
This joint is comprised of several components that work together seamlessly. The main components of the TMJ include the condyle of the mandible, which fits into a socket called the glenoid fossa, located in the temporal bone of the skull. To further stabilize the joint, there is a layer of fibrocartilage known as the articular disc, which acts as a cushion between the condyle and the glenoid fossa. Surrounding the joint, there are several groups of muscles, ligaments, and tendons that provide support and enable the smooth movement of the TMJ. When all these components are functioning properly, the TMJ works harmoniously to facilitate normal mouth movements.
Common causes of TMD
Temporomandibular Joint Disorder, or TMD, can be caused by a variety of factors. One common cause is trauma to the jaw joint or the muscles surrounding it. This can occur due to a blow to the face, a car accident, or any other incident that puts stress on the temporomandibular joint (TMJ). Additionally, TMD can be triggered by the misalignment of the teeth or the jaw, also known as malocclusion. When the upper and lower teeth don’t fit together properly, it can put excessive strain on the TMJ, leading to discomfort and pain. Other causes of TMD include arthritis, which can cause inflammation and damage to the joint, and bruxism, or teeth grinding, which can put excessive pressure on the TMJ and the surrounding muscles. Identifying the underlying cause of TMD is crucial in determining the appropriate treatment approach.

A less common but noteworthy cause of TMD is stress. While stress itself doesn’t directly cause TMD, it can contribute to the development or exacerbation of its symptoms. When we are stressed, we tend to clench our teeth or tighten our jaw muscles, leading to muscle tension and discomfort in the TMJ area. Furthermore, stress can also lead to behaviors such as teeth grinding or nail biting, which can put additional strain on the TMJ. It’s important to address and manage stress as part of a comprehensive treatment plan for TMD.
How does stress impact TMD?
Stress is a common factor that can greatly impact temporomandibular joint disorder (TMD). When we experience stress, it can lead to increased muscle tension, particularly in the jaw area. This tension can put additional strain on the temporomandibular joint (TMJ), exacerbating the symptoms of TMD.
Research has shown that individuals who are experiencing high levels of stress are more likely to report symptoms of TMD, such as jaw pain, headaches, and difficulty chewing. The exact mechanism by which stress affects TMD is not fully understood, but it is believed that stress hormones and neurotransmitters may play a role in altering muscle activity and sensitivity in the jaw.
It is important to note that while stress can contribute to the development and progression of TMD, it is not the sole cause. TMD is a multifactorial condition, and other factors, such as genetics, trauma, and dental occlusion, can also influence its onset and severity. Understanding and managing stress levels, along with addressing other contributing factors, is crucial in effectively managing TMD and improving overall oral health.

Recognizing the symptoms of TMD
TMD, or Temporomandibular Joint Disorder, is a condition that affects the jaw joint and surrounding muscles. Recognizing the symptoms of TMD is crucial in order to seek appropriate treatment and manage the discomfort it may cause. Common symptoms include jaw pain or tenderness, difficulty opening or closing the mouth, clicking or popping sounds when moving the jaw, and facial pain that radiates to the neck or shoulders.
In addition to these primary symptoms, individuals with TMD may also experience headaches, earaches, and pain or pressure behind the eyes. It is important to note that the severity and frequency of these symptoms can vary from person to person. Some individuals may find their symptoms to be transient and manageable, while others may experience persistent and debilitating discomfort. If you are experiencing any of these symptoms, it is advisable to consult with a healthcare professional or a dentist who specializes in TMD for a thorough evaluation and appropriate management.
The link between TMD and teeth grinding
Teeth grinding, also known as bruxism, is a common habit that can often be associated with temporomandibular joint disorder (TMD). While not all individuals who grind their teeth will develop TMD, the two conditions can have a reciprocal relationship. Studies have shown that teeth grinding can be both a cause and a consequence of TMD, making it important to address this habit in the management of TMD.
When it comes to the link between TMD and teeth grinding, it is believed that the excessive force exerted during grinding can disrupt the delicate balance of the temporomandibular joint. Over time, this repetitive motion can lead to inflammation, muscle soreness, and structural changes in the joint, exacerbating TMD symptoms. Conversely, individuals with TMD may unintentionally develop the habit of teeth grinding as a subconscious attempt to alleviate discomfort or find relief from the associated pain.
| Aspect | Temporomandibular Joint Disorder (TMD) | Teeth Grinding (Bruxism) |
|---|---|---|
| Definition | Dysfunction of the jaw joint | Involuntary clenching or grinding of teeth |
| Symptoms | Jaw pain, clicking or popping sounds in the jaw, difficulty chewing, facial pain, headaches | Tooth wear, jaw muscle discomfort, headaches, earaches |
| Causes | Trauma to the jaw, arthritis, excessive stress on the jaw joint, misalignment of teeth or jaw | Stress, anxiety, sleep disorders, abnormal bite |
| Relationship | Bruxism can contribute to TMD by placing excessive pressure on the jaw joint and muscles | TMD can exacerbate bruxism due to pain or discomfort, leading to compensatory teeth grinding |
| Treatment | Stress management, jaw exercises, oral splints, physical therapy, medications | Mouthguards or splints to protect teeth, stress reduction techniques, addressing underlying sleep disorders, muscle relaxants |
Understanding the connection between TMD and teeth grinding highlights the significance of addressing both aspects when it comes to treatment and management. By effectively managing teeth grinding, through the use of oral appliances such as mouth guards or splints, the excessive forces on the joint can be reduced, potentially alleviating TMD symptoms. Similarly, addressing and managing TMD can help minimize the occurrence and severity of teeth grinding, providing relief to individuals affected by this condition.
Can poor posture contribute to TMD?
Poor posture can indeed contribute to temporomandibular joint disorder (TMD). The temporomandibular joint (TMJ) is closely connected to the alignment of the head, neck, and spine. When posture is poor, it can result in misalignment and increased pressure on the TMJ, leading to the development or exacerbation of TMD symptoms.
Maintaining proper posture helps ensure the correct alignment of the jaw joint and reduces the strain on the muscles involved in chewing and jaw movement. Slouching or holding the head in a forward position, common in individuals who sit for extended periods or use electronic devices frequently, can alter the natural alignment of the jaw joint and lead to muscle imbalances. These imbalances can contribute to painful symptoms such as jaw pain, clicking or popping sounds, limited jaw movement, and headaches.
Improving posture through exercises, ergonomic adjustments, and conscious awareness of body positioning can help alleviate TMD symptoms. It is important to seek professional help to identify and address any posture-related issues that may be contributing to TMD. A dentist or other healthcare provider with expertise in TMD can provide guidance on improving posture and offer treatment options to relieve symptoms and promote better oral health.
The role of genetics in TMD development
Research suggests that genetics can play a role in the development of Temporomandibular Joint Disorder (TMD). Studies have found that individuals with a family history of TMD are more likely to be affected by the condition themselves. In fact, a study conducted on twins found that identical twins, who share the same genetic makeup, were more likely to both have TMD compared to non-identical twins. These findings indicate that there may be a genetic predisposition to TMD, although the specific genes involved have not yet been identified.
While genetics may contribute to the development of TMD, it is important to note that other factors, such as environmental and lifestyle factors, can also play a significant role. For example, individuals with a family history of TMD may be more susceptible to developing the condition if they engage in habits that can place strain on the temporomandibular joint, such as teeth grinding or clenching. Additionally, certain environmental factors, such as trauma or injury to the jaw, can further contribute to the development of TMD. Further research is needed to fully understand the complex interplay between genetics and environmental factors in TMD development.
Diagnosing TMD: What to expect during an evaluation
During an evaluation for temporomandibular joint disorder (TMD), your dentist or oral health professional will carefully examine your jaw, teeth, and surrounding structures to assess the extent of your condition. The evaluation process typically involves a comprehensive medical and dental history review, where you will be asked about any symptoms you may be experiencing, previous dental treatments, and any relevant medical conditions.
In addition, your dentist will perform a thorough physical examination of the jaw joint and surrounding muscles. This may include checking for tenderness, clicking or popping sounds, limited range of motion, and any abnormalities in the bite. X-rays or other imaging tests may also be ordered to get a more detailed view of the joint and ruling out other potential causes of your symptoms. Overall, the evaluation process aims to gather all the necessary information to make an accurate diagnosis and develop an appropriate treatment plan tailored to your specific needs.
The different types of TMD treatment options available
TMD, or temporomandibular joint disorder, can cause significant discomfort and hinder everyday activities like eating or speaking. Fortunately, there are various treatment options available to alleviate the symptoms and improve the quality of life for individuals with TMD.
One common approach in managing TMD is conservative, non-invasive treatments. This may include self-care practices such as applying heat or cold packs to the affected area, practicing relaxation techniques to reduce stress, and avoiding activities that exacerbate symptoms. Additionally, physical therapy and exercises tailored to strengthen the muscles and improve flexibility in the jaw joint may be recommended. These non-surgical interventions aim to relieve pain, reduce inflammation, and enhance the overall function of the temporomandibular joint.
In cases where conservative treatments do not provide sufficient relief, more advanced interventions may be considered. Oral splints or mouth guards, for example, can be custom-made to fit over the teeth and provide stability to the jaw joint. These devices help alleviate pressure on the joint and promote proper alignment of the jaw. Surgical options may also be explored for severe or persistent TMD cases. These procedures range from arthrocentesis, a minimally invasive technique that flushes out inflammatory substances within the joint, to joint replacement for more severe and debilitative conditions.
| Treatment Option | Description |
|---|---|
| Self-Care/Home Remedies | – Resting the jaw by avoiding chewing gum or tough foods |
| – Applying ice packs or moist heat to the jaw area for pain relief | |
| – Practicing relaxation techniques such as meditation or yoga to reduce stress | |
| – Performing jaw exercises to improve flexibility and strengthen muscles | |
| Medications | – Over-the-counter pain relievers such as ibuprofen or acetaminophen |
| – Muscle relaxants prescribed by a doctor to relieve muscle spasms | |
| – Tricyclic antidepressants or other medications to manage chronic pain and improve sleep | |
| – Injections of corticosteroids or Botox to reduce inflammation and muscle tension | |
| Dental Treatments | – Dental splints or mouthguards to reduce teeth grinding and clenching during sleep |
| – Orthodontic treatment to correct bite misalignment or malocclusion | |
| – Dental restorations such as crowns or bridges to correct bite abnormalities | |
| – Tooth extraction in severe cases where misaligned teeth are causing TMD symptoms | |
| Physical Therapy | – Jaw exercises and stretches to improve range of motion and reduce muscle tension |
| – Manual therapy techniques such as massage or manipulation to relieve pain and stiffness | |
| – Ultrasound or electrical stimulation to promote healing and reduce inflammation | |
| – Posture correction and ergonomic advice to alleviate strain on the jaw joint and muscles | |
| Lifestyle Changes | – Avoiding hard or chewy foods that can exacerbate symptoms |
| – Limiting caffeine and alcohol intake, as they can increase muscle tension and worsen pain | |
| – Using relaxation techniques and stress management strategies to reduce jaw clenching and tension | |
| Surgical Options | – Arthrocentesis, a minimally invasive procedure to flush out debris or inflammatory fluids from the joint |
| – Arthroscopy to repair or remove damaged tissue within the joint | |
| – Open joint surgery for severe cases of joint degeneration or structural abnormalities | |
| – Joint replacement as a last resort for irreversible joint damage |
It is important to note that the most appropriate treatment option for each individual depends on factors such as the severity of symptoms, the underlying cause of TMD, and the patient’s overall health. A thorough evaluation by a qualified healthcare professional, such as a dentist or oral and maxillofacial surgeon, is essential to determine the most suitable course of action. Seeking professional help ensures that individuals receive personalized and effective treatment to manage their TMD symptoms successfully.
Medications commonly used to manage TMD symptoms
Medications play a crucial role in managing the symptoms of Temporomandibular Joint Disorder (TMD) and can provide relief to individuals experiencing pain and discomfort. There are several types of medications commonly used to alleviate TMD symptoms, with the choice of medication depending on the severity and specific symptoms experienced by the patient.
One common medication used for TMD symptom management is nonsteroidal anti-inflammatory drugs (NSAIDs). These medications, such as ibuprofen or naproxen sodium, work by reducing inflammation and relieving pain. NSAIDs can be effective in reducing the swelling and discomfort associated with TMD, allowing individuals to experience temporary relief from their symptoms. However, it is important to note that long-term use of NSAIDs should be done under the guidance of a healthcare professional due to potential side effects.
Non-surgical interventions for TMD: Physical therapy and exercises
Physical therapy and exercises may be recommended as non-surgical interventions for individuals with temporomandibular joint disorder (TMD). These interventions aim to improve the function and strength of the jaw muscles, reduce pain and inflammation, and restore normal range of motion.
Physical therapy for TMD often involves a combination of stretching and strengthening exercises, along with techniques to improve posture and body mechanics. These exercises are designed to target the muscles involved in jaw movement and help alleviate muscle tension and imbalances that contribute to TMD symptoms. Specific exercises may include gentle jaw opening and closing movements, isometric exercises to strengthen the jaw muscles, and stretching exercises for the neck, shoulders, and facial muscles.
Under the guidance of a trained physical therapist, patients learn proper techniques and are educated on self-management strategies that can help mitigate pain and discomfort associated with TMD. The therapist may also incorporate modalities such as heat or cold therapy, ultrasound, or electrical stimulation to provide additional pain relief and accelerate the healing process. Additionally, patients may receive instruction on relaxation techniques and stress reduction methods, as stress can exacerbate TMD symptoms.
The potential benefits of using oral splints or mouth guards
Oral splints and mouth guards are commonly used in the management of Temporomandibular Joint Disorder (TMD). These oral appliances are designed to help alleviate the symptoms associated with TMD and promote healing of the jaw joint.
One of the main benefits of using oral splints or mouth guards is their ability to provide a protective barrier between the upper and lower teeth. This helps to prevent further damage to the teeth and jaw joint caused by grinding or clenching, which are commonly associated with TMD. By creating a cushioning effect, these devices absorb the forces exerted during teeth grinding or clenching, reducing the risk of tooth wear, fractures, and jaw joint damage.
Furthermore, oral splints and mouth guards can help to stabilize the jaw joint by promoting proper alignment and reducing excessive movement. By repositioning the jaw into a more favorable position, these devices can help relieve muscle tension and strain, alleviating symptoms such as facial pain, headaches, and difficulty in opening or closing the mouth. The use of oral splints or mouth guards can also help to redistribute forces across the jaw joint, reducing the load on specific areas and promoting an overall more balanced bite.
Surgical options for severe or persistent TMD cases
For severe or persistent cases of Temporomandibular Joint Disorder (TMD), surgical options may be considered as a last resort when other conservative treatments have proven ineffective. Surgery aims to repair or correct structural issues within the temporomandibular joint (TMJ) that are causing the TMD symptoms.
One surgical option is arthroscopy, a minimally invasive procedure that allows the surgeon to examine and treat the TMJ using a small camera and specialized instruments inserted through tiny incisions. Arthroscopy can help remove adhesions, repair damaged tissues, or correct structural abnormalities that may be contributing to TMD. In more severe cases, open joint surgery may be necessary, involving the repositioning or replacement of the TMJ disc, the removal of damaged joint tissues, or the realignment of the jaw joint. Surgical procedures, such as arthroplasty or joint replacement, may also be considered in rare cases where the joint is significantly damaged and cannot be salvaged through other means.
Lifestyle changes and self-care practices to alleviate TMD symptoms
Implementing lifestyle changes and self-care practices can play a crucial role in alleviating the symptoms associated with Temporomandibular Joint Disorder (TMD). Alongside professional treatment, these strategies can enhance the overall management of TMD and promote improved oral health.
One key lifestyle change to consider is adopting a diet that supports jaw health. Opting for softer foods that require less chewing can help reduce the strain on the temporomandibular joint (TMJ). Additionally, avoiding hard, sticky, or excessively chewy foods can lessen discomfort and prevent further aggravation of TMD symptoms. It is advisable to incorporate a balanced diet rich in essential nutrients, such as calcium and vitamin D, which support healthy bone and muscle function.
In addition to dietary modifications, practicing stress management techniques can have a positive impact on TMD symptoms. Stress has been linked to jaw clenching and teeth grinding, commonly associated with TMD. Techniques such as deep breathing exercises, meditation, and yoga can help relax the jaw muscles and minimize tension. Engaging in regular physical exercise and getting an adequate amount of sleep can also help reduce stress levels, contributing to the overall improvement of TMD symptoms.
The importance of seeking professional help for TMD management.
Seeking professional help for the management of Temporomandibular Joint Disorder (TMD) is crucial for individuals experiencing its symptoms. TMD is a complex condition that requires a thorough evaluation and tailored treatment plan. Dentists, specifically those skilled in TMD diagnosis and treatment, possess the expertise necessary to address the unique needs of each patient.
Professional assistance is essential for accurately diagnosing TMD. Dentists who specialize in TMD management possess the knowledge and skills to conduct a comprehensive evaluation, which includes a detailed medical history, physical examination, and assessment of the temporomandibular joint (TMJ) function. Through their expertise, they can differentiate TMD from other conditions that may present similar symptoms.
Once a diagnosis has been established, seeking professional help ensures the implementation of appropriate treatment strategies. Dentists experienced in managing TMD can recommend a range of interventions, tailored to the individual’s specific condition and needs. These may include lifestyle modifications, physical therapy, oral splints or mouth guards, medication, or, in severe cases, surgery. Professional guidance is pivotal in determining the most effective course of action to alleviate symptoms, improve jaw function, and enhance overall quality of life.
In conclusion, the importance of seeking professional help for TMD management cannot be overstated. Dentists specializing in TMD possess the necessary expertise to accurately diagnose the condition and implement suitable treatment approaches. By entrusting their care to these professionals, individuals with TMD can achieve symptom relief, improved jaw function, and an enhanced overall oral health and well-being.
What is Temporomandibular Joint Disorder (TMD)?
Temporomandibular Joint Disorder (TMD) refers to a condition that affects the jaw joint and surrounding muscles, causing pain, discomfort, and difficulty in jaw movement.
How does stress impact TMD?
Stress can worsen the symptoms of TMD as it leads to increased muscle tension in the jaw and face, exacerbating pain and discomfort.
Can poor posture contribute to TMD?
Yes, poor posture can contribute to TMD by placing strain on the muscles and joints of the jaw, leading to pain and dysfunction.
What role does genetics play in TMD development?
While the exact cause of TMD is not fully understood, genetics may play a role in its development. Certain genetic factors can make individuals more prone to developing TMD.
How is TMD diagnosed?
TMD can be diagnosed through a comprehensive evaluation by a healthcare professional, which may include a physical examination, review of medical history, and possibly imaging tests.
What are the non-surgical interventions for TMD?
Non-surgical interventions for TMD may include physical therapy, exercises, and the use of oral splints or mouth guards to reduce pain and improve jaw function.
When are surgical options considered for TMD?
Surgical options for TMD are typically considered in severe or persistent cases where conservative treatments have not provided satisfactory relief.
What lifestyle changes can alleviate TMD symptoms?
Lifestyle changes such as managing stress levels, practicing relaxation techniques, maintaining good posture, avoiding hard or chewy foods, and avoiding habits like teeth clenching or grinding can help alleviate TMD symptoms.
How can seeking professional help benefit TMD management?
Seeking professional help for TMD management is important because healthcare professionals can provide an accurate diagnosis, recommend appropriate treatment options, and guide individuals in managing their symptoms effectively.











